Paid online consultations are available by appointment. For booking, please contact us via Whatsapp.
Metastatic Brain Tumors: Comprehensive Diagnosis, Treatment, and Survival Guide
Receiving a cancer diagnosis is undoubtedly one of the most challenging turns in your life. Honestly, hearing terms like “spread to the brain” or medically “brain metastasis” during treatment causes deep anxiety. It might even terrify you. However, do not despair immediately. Because modern medicine has made incredible progress in this field, especially in the last decade. Therefore, we no longer view metastatic brain tumors as a hopeless end. On the contrary, we accept them as a manageable chronic condition with the right planning.
For this reason, take a deep breath and calm down. We are by your side with our advanced technology, surgical experience, and oncology team. Specifically, we prepared this comprehensive guide so you can find clear answers to questions like “Why me?”, “Can I recover?”, or “Is surgery necessary?”. Thus, you will understand the disease in detail and start the treatment process stronger and more conscious.
What is a Metastatic Brain Tumor?
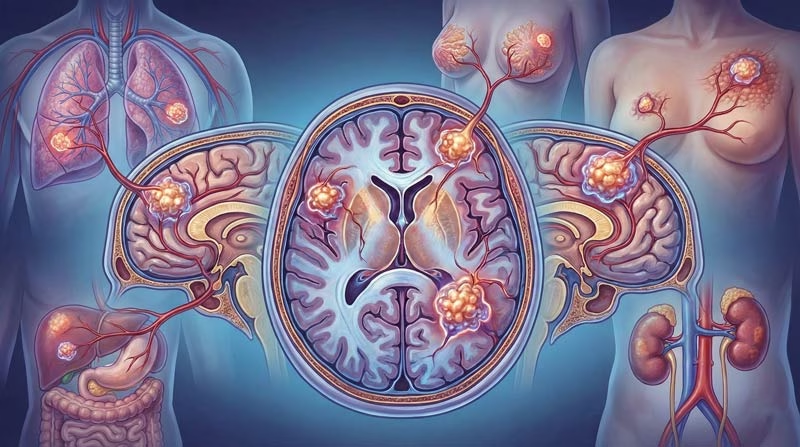
Metastatic brain tumors do not originate from the brain’s own nerve cells. In contrast, cancerous cells from a completely different part of the body (such as the lung, breast, or kidney) initiate this problem. These aggressive cells detach from their original organ. Subsequently, they leak into the bloodstream. They take a long journey through the blood and reach the brain. Finally, they latch onto the vascular structure there and settle. In short, we physicians call these “secondary tumors” or “guest tumors.”
Interestingly and surprisingly, these tumors are much more common than primary brain tumors (those originating in the brain). So, when we see a mass in the brain, statistically, the possibility of metastasis comes to mind first. Despite this, do not act with fear. Because as multidisciplinary tumor boards, oncology, and neurosurgery teams, we work together. Thus, we successfully manage this complex process.
Summary: Understand the Disease in 5 Points
Your time might be limited, or you might be overwhelmed by intense medical information. Therefore, we have summarized the most critical points for you to grasp the essence of the subject quickly:
- Propagation Route: Cancer cells use blood vessels, the body’s highways, to travel to the brain.
- Main Sources: Especially lung cancer and breast cancer are the types that metastasize to the brain most frequently.
- Appearance: Sometimes we see a single large mass in the brain, and sometimes multiple small foci scattered around.
- Modern Solutions: Microsurgery, targeted smart drugs, and point-shot radiation therapies (Radiosurgery) save lives.
- Critical Warnings: You experience severe headaches increasing in the morning, sudden seizures, and weakness on one side of the body.
How Does It Form? The Journey of the Cell
So, how exactly does this process develop? Understanding this is important for grasping the logic of treatment. The tumor in the body grows uncontrollably. When it reaches a certain size, it creates its own vascular structure. However, this structure is weak. Consequently, cancer cells break off from here and mix into the blood. The brain is the body’s most blood-supplied organ. Approximately 20% of the blood leaving the heart goes directly to the brain. For this reason, unfortunately, the brain is a frequent stop for cancer cells circulating in the blood.
Moreover, there is a protective filter in the brain called the “Blood-Brain Barrier.” We used to think this barrier stopped cancer. However, aggressive cells breach this barrier. Furthermore, once they get inside, this barrier sometimes makes it difficult for drugs (chemotherapy) to enter. That is why we surgeons and radiation oncologists prioritize planning local treatments directed specifically at the brain.
Which Cancers Reach the Brain?
Biologically, the body carries the potential to send almost every type of cancer to the brain. However, statistics show us that some cancer types love going to the brain more. For example, according to our clinical experiences and scientific data, we encounter the following most frequently:
1. Lung Cancer
It leads the list by a wide margin. In fact, about half of the patients diagnosed with lung cancer experience this situation at some stage of their disease. Sometimes the patient does not know they have a problem in their lungs at all. They come to us directly with complaints of headache or seizure. As a result of tests, we find the main focus in the lung.
2. Breast Cancer
It is the second most common cause we encounter in female patients. Particularly in subtypes we call HER2 positive or Triple Negative, the risk of spreading to the brain increases. On the other hand, breast cancer treatment has created a revolution in recent years. Thanks to current drugs and treatments, these patients live a quite long and high-quality life.
3. Melanoma (Skin Cancer)
It is the most aggressive and dangerous type of skin cancer. Unfortunately, it tends to cause bleeding brain tumors. For this reason, if you have a history of melanoma or a suspicious mole removal procedure, you should take even the slightest headache seriously.
4. Kidney and Colon Cancers
Although seen less frequently, kidney (renal cell) and large intestine tumors also metastasize to the brain. Especially those originating from the kidney respond quite well to surgery.
Symptoms by Region and Warning Signs
The moment the tumor settles in the brain, it increases the pressure inside that closed box of the skull. At the same time, it presses on the sensitive nerve networks in its region. Our brain is like a map; every region manages a different job. Consequently, your body sends you different emergency signals depending on the location of the tumor:
General Intracranial Pressure Symptoms
- Persistent Headache: It differs from ordinary tension-type pains. Especially you feel it very severely when you wake up in the morning or when you cough and strain.
- Nausea and Vomiting: You experience unexplained, projectile vomiting. It usually accompanies the headache.
- Seizure (Epilepsy): If you are an adult and have a seizure out of nowhere for the first time in your life, this situation screams by 90% that there is a mass in your brain.
Regional (Focal) Symptoms
- Frontal Lobe (Front Area): If the tumor is here, you experience personality changes. You become more irritable, indifferent, or forgetful. Your decision-making ability deteriorates.
- Parietal Lobe (Side Area): You lose your sense of direction. You confuse your right and left. You struggle with reading and writing.
- Temporal Lobe (Temple Area): Memory problems begin. You might smell odors that don’t exist. You have difficulty understanding what is spoken.
- Occipital Lobe (Back Area): Your vision center is here. You might lose half of your visual field. Flashing lights might appear before your eyes.
- Cerebellum: This is your balance center. You start walking unsteadily like you are drunk. You experience tremors when reaching for an object with your hand.
Important note: Experiencing one or several of these symptoms does not mean you definitely have cancer. However, we strongly recommend that you do not let your guard down and see a neurosurgeon without wasting time.
Diagnosis: Advanced Imaging
When you come to our clinic anxiously, firstly, we calm you down and listen to your complaints in detail. Then, we perform a neurological examination that measures your reflexes, fundus of the eye, and muscle strength. But to make a definitive decision, we need to see inside the brain with our own eyes. Therefore, we use advanced imaging technologies:
Contrast-Enhanced Brain MRI (Magnetic Resonance)
We rely on this the most when diagnosing. It is the gold standard. We administer a special drug called “contrast agent” through your arm vein. Then we take you to the MRI device. Thanks to this drug, tumor tissues in the brain appear in bright white color as if saying “I am here.” Thus, we surgeons clearly see the number of tumors, their millimetric size, their proximity to sensitive areas, and the amount of edema.
Computed Tomography (CT)
If you have a pacemaker or metal prosthesis in your body that is not MRI-compatible, you cannot have an MRI. In this case, we prefer the Tomography method. Also, CT is very valuable for understanding whether the tumor damages the bone structure.
PET-CT Scan (Whole Body)
Sometimes our patient comes to us with a brain tumor; however, we do not know where else in the body the cancer is. Here, we track traces like a detective. With PET-CT, we scan the whole body from head to toe. We administer a drug marked with a sugary substance. Since cancer cells love sugar very much, they hold this drug and shine. Thus, we identify the “main source” (primary focus).
Treatment Plan: Surgery and Medication
Every patient’s story, genetics, and resistance are different. Therefore, instead of a “standard” treatment, we draw a “personalized” plan. When making this decision, we lay these questions on the table: How many tumors are there? Where does it stand in the brain? How is our patient’s age and general performance? Is the main cancer under control?
1. Surgical Treatment (Microsurgery)
If the tumor is a single focus, large in size (over 3-4 cm), and putting serious pressure on your brain, we choose surgery. Because our primary goal here is to remove that mechanical pressure and relieve the patient.
With microsurgical methods, we work under high-magnification microscopes. Without touching the healthy brain tissue even by a millimeter, we peel the tumor off the vessels and nerves and remove it. Thanks to the “Brain GPS” we call Neuronavigation, we do not lose our way. After surgery, intracranial pressure drops. Thereby, the risk of paralysis decreases, and our patient’s consciousness improves rapidly. Additionally, we send the removed piece for genetic analysis. Afterwards, oncologists arrange your smart drug treatment accordingly.
2. Whole Brain Radiation Therapy (WBRT)
We used to use it very frequently. However, due to side effects (forgetfulness, dizziness), we behave more selectively now. If there are widespread metastases in the brain too numerous to count (for example, 10-15), we irradiate the whole brain at a low dose. Our goal is to brake the disease.
Knife-less Surgery: Gamma Knife
Perhaps you are afraid of surgery, scalpels, or anesthesia. Or your tumor is at a point too sensitive and deep to be operated on. In that case, we have great news for you: Stereotactic Radiosurgery (Gamma Knife / CyberKnife). In this technology, we do not use a knife, we do not cut your scalp, we do not shed blood.
- How Do We Do It? We fix your head with a special frame or mask. We make millimetric planning on the computer. Then, we direct high-energy beams coming from nearly 200 sources to a single focal point.
- What is the Effect? These beams do not damage the brain while going to the target. However, they create enormous energy at the point where they converge (inside the tumor). This energy disrupts the tumor’s DNA and kills it. Ultimately, the tumor shrinks over time and turns into scar tissue in its place.
- Who Do We Apply It To? It is the gold standard especially for tumors smaller than 3 cm and few in number (between 1-4).
- Advantage: The procedure is performed on an outpatient basis. You come in the morning, your procedure is done, and you can drink your tea at home in the afternoon. Your hair does not fall out.
Smart Drugs and Support Treatments
Just removing the tumor is not enough. We must win the war in the body totally. In the past, chemotherapy drugs could not reach the brain much. Because the brain would not let the drugs in to protect itself. However, medical technology has changed.
We now use “Smart Drugs” (Targeted Therapies). These molecules are so small that they cross the wall in the brain. They find the cancer cell directly and stick to it. Also, with the method we call “Immunotherapy,” we train the body’s own immune system. Thus, your own soldiers attack the cancer.
Support Treatments: We start cortisone treatment to reduce the edema (swelling) caused by the tumor. This stops your headache quickly. If you have a risk of seizures, we add anti-seizure medications. You must use these drugs regularly until your doctor says stop.
Frequently Asked Questions (FAQ)
How long does a patient with brain metastasis live?
Our patients and their relatives ask this question frequently and with anxiety. However, to be honest, giving a definite time is not scientific and would not be correct. Because every body, every tumor reacts differently. Nevertheless, know this clearly: Forget the old statistics. Thanks to smart drugs, immunotherapy, and Gamma Knife technology, our patients now live a high-quality life expressed in years, not months. In fact, there are many patients who continue their lives with complete recovery.
Is surgery risky?
Of course, there is no such thing as “zero risk” in medicine. Every procedure has its own risks. But metastatic tumors do not take root into the tissue like the brain’s own tumors. They usually have a capsule and push the brain tissue. This situation makes our job relatively easier surgically. Moreover, we minimize the margin of error with neuromonitoring and navigation technologies we use during surgery.
Does the tumor go away completely, does it recur?
As surgeons, we clean the visible tumor completely. However, cells hiding at the microscopic level may remain. That is why we definitely add radiation therapy after surgery. Still, cancer is stubborn by nature and may recur. Therefore, you should never skip the MRI controls we will do at 3-6 month intervals. If we catch it early, we always have a chance to intervene again.
How should nutrition be?
Body resistance is very important in the fight against cancer. You should eat a protein-rich diet. You should stay away from sugary foods and processed products. However, do not believe in unscientific promises saying “if you eat this, the tumor will disappear.” Do not use any herbal cures without consulting your doctor; because these herbs can interact with your chemotherapy drugs and cause your liver to fail.
Important Warning: We wrote this comprehensive guide to inform and guide you. Please do not settle for internet information for diagnosis, treatment, and medication use. Definitely consult a specialist neurosurgeon or oncologist. Your health is more valuable to us than anything.
For more detailed scientific data and current studies, you can browse international sources: Cleveland Clinic – Brain Tumors and Johns Hopkins Medicine
Ready to Take the Next Step?
Schedule your consultation with Dr. Albayrak today and start your journey towards better health.




