Paid online consultations are available by appointment. For booking, please contact us via Whatsapp.
Myelomeningocele (Spina Bifida)
Facing a myelomeningocele diagnosis? Learn about advanced surgical treatments and lifelong care from leading neurosurgeon Prof. Dr. Serdar Baki Albayrak in Turkey.
- On
- InUncategorized
A Comprehensive Guide to Myelomeningocele (Spina Bifida): Diagnosis, Expert Surgery, and Lifelong Care
Receiving a diagnosis of myelomeningocele for your child can feel overwhelming. You are not alone. With timely, expert surgery and coordinated follow‑up, many children achieve meaningful improvements in function and quality of life. This page offers clear, trustworthy, and hopeful guidance from our pediatric neurosurgery team led by Prof. Dr. Serdar Baki Albayrak.
Last reviewed: 17 August 2025 • Evidence‑based content • Patient‑centered language
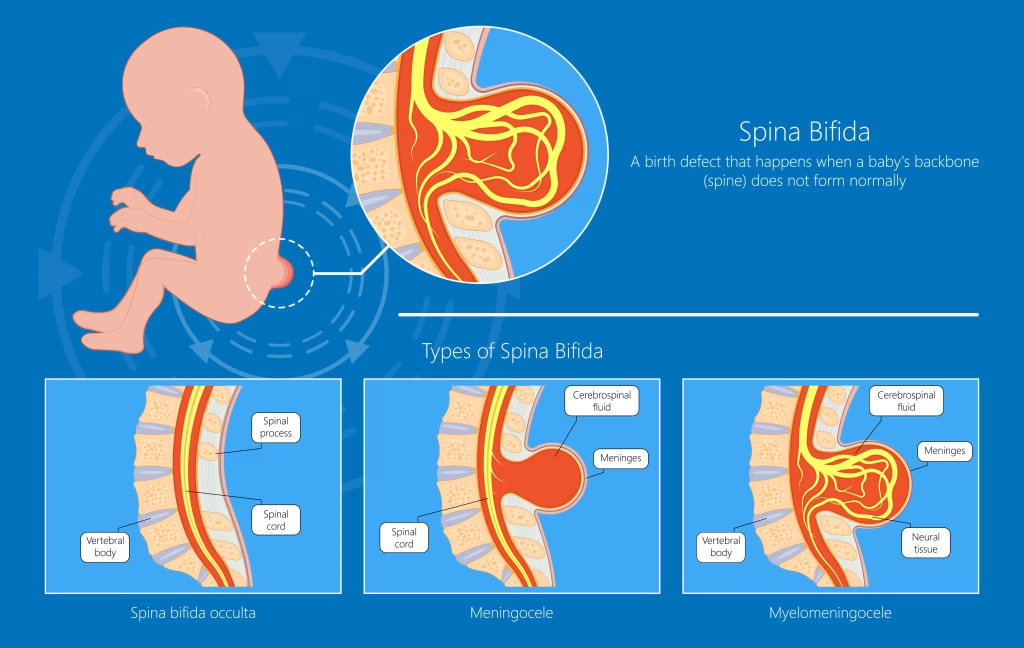
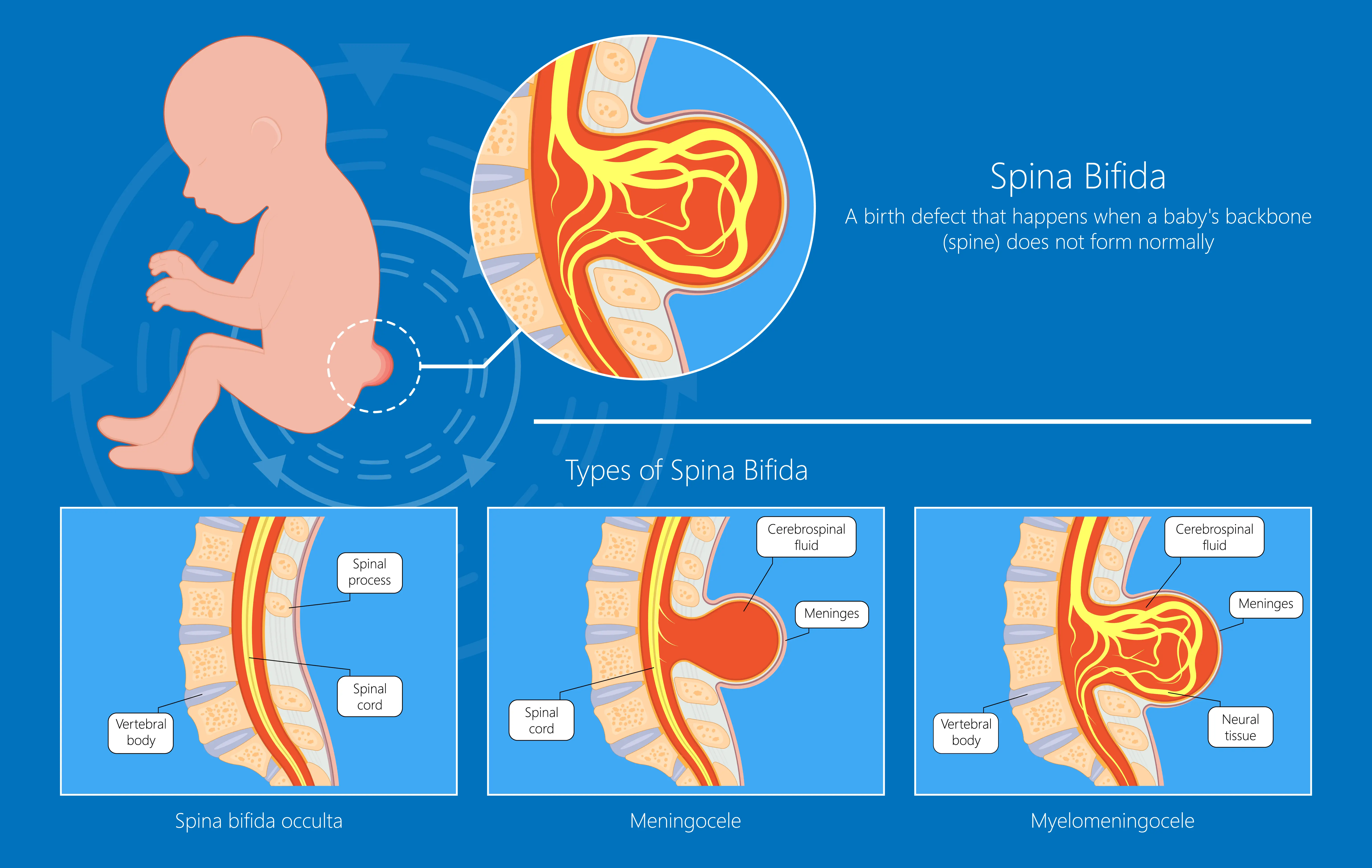
What is Myelomeningocele? Understanding Open Spina Bifida
Myelomeningocele is a neural tube defect in which the spinal cord and its protective membranes (meninges) protrude through an opening in the spine, usually visible as a sac on the newborn’s back. Because the spinal cord is involved, neurological symptoms are typically more significant than in other forms of spina bifida.
How it differs from other types: In meningocele, only the meninges herniate without spinal cord involvement; in spina bifida occulta, the defect is closed and often discovered incidentally.
Common signs and symptoms
- Lower limb weakness or paralysis
- Bladder and bowel control difficulties
- Orthopedic issues (e.g., clubfoot, hip instability)
- Associated conditions such as hydrocephalus and Chiari II malformation
Prenatal and Postnatal Diagnosis of Myelomeningocele
Prenatal diagnosis
- Alpha‑fetoprotein (AFP) test: Elevated maternal serum AFP can suggest a neural tube defect.
- Ultrasound: Targeted fetal ultrasound visualizes the spinal defect and related findings.
- Amniocentesis: In selected cases, used to support diagnosis and counseling.
Postnatal diagnosis
- Physical examination identifies the back lesion at birth.
- Imaging (e.g., MRI) defines the level of the lesion and associated anomalies.
The Critical Importance of Myelomeningocele Surgery After Birth
Early repair—usually within the first 24–72 hours of life—reduces infection risk and helps protect exposed neural tissue.
Goals of myelomeningocele repair
- Prevent infection (e.g., meningitis)
- Protect the spinal cord from further injury
- Return neural elements to the spinal canal and close the defect in layers
The surgical procedure: Our microsurgical approach
Using operating microscopes and meticulous microsurgical technique, the neural tissue is gently repositioned. Dura, muscle, and skin are closed in layers to achieve a watertight closure. Anesthesia, neonatology, and pediatric urology teams coordinate perioperative care.
Managing Associated Conditions: Hydrocephalus and Chiari II Malformation
Hydrocephalus is common and may be treated with a ventriculoperitoneal (VP) shunt or other CSF diversion procedures. Learn more: Hydrocephalus – Causes & Treatment.
Chiari II malformation can affect breathing or swallowing. Management is individualized and may include decompression surgery or supportive therapies.
If indicated, we also evaluate for tethered spinal cord during follow‑up.
External resources for families: Spina Bifida Association · WHO – Neural Tube Defects
Life After Surgery: Long‑Term Outlook and Multidisciplinary Care
Surgery is the beginning of care. With a coordinated plan, many children thrive.
- Physiotherapy & rehabilitation: Mobility, balance, and strength training.
- Urology care: Bladder and bowel programs, clean intermittent catheterization when needed.
- Orthopedics: Management of foot, hip, or spine issues; bracing or surgery as needed.
Can a child with myelomeningocele walk?
Walking potential depends on the lesion level and muscle function. Some children walk independently; others use braces, crutches, or wheelchairs. Early rehab maximizes function.
Why Choose Prof. Dr. Serdar Baki Albayrak for Spina Bifida Treatment in Turkey?
- Experience: Extensive pediatric neurosurgery practice, including complex myelomeningocele repairs.
- Technology: Advanced microscopes and neuro‑monitoring tailored to neonatal care.
- Multidisciplinary model: Close collaboration with neonatology, pediatric urology, orthopedics, and physiotherapy.
- International patients: Dedicated coordinators for travel, translation, and continuity of care.
Learn more about our service line: Pediatric Neurosurgery · Meet the surgeon: Prof. Dr. Serdar Baki Albayrak.
Frequently Asked Questions
What is the life expectancy for a child with myelomeningocele?
With modern surgical care and coordinated follow‑up, many individuals live into adulthood with good quality of life. Prognosis varies by lesion level and associated conditions.
Is surgery a cure for spina bifida?
Surgery closes the defect and protects the spinal cord but does not reverse pre‑existing nerve injury. Ongoing therapies and monitoring are essential.
What therapies will my child need after surgery?
Most children benefit from physiotherapy, occupational therapy, pediatric urology follow‑up, and tailored orthopedic support.
How can we manage bladder and bowel problems?
Clean intermittent catheterization, medications, and bowel management plans are common strategies guided by pediatric urology.
Ready to talk to an expert?
If your child has been diagnosed with spina bifida myelomeningocele, a timely consultation with a pediatric neurosurgeon is crucial. Our team is here to guide you.
Book an AppointmentPrefer to speak now? Visit our Contact page for phone and WhatsApp options.