Paid online consultations are available by appointment. For booking, please contact us via Whatsapp.

What is Craniopharyngioma?
Facing a brain tumor diagnosis is undoubtedly tough. For instance, as a patient or relative, you are likely living through a challenging moment. Currently, you hold an MRI report in your hand. Specifically, it says “Craniopharyngioma”. Consequently, you search the internet immediately. However, complex terms appear on your screen. Therefore, worrying is perfectly normal. Nevertheless, take a deep breath now. Above all, do not panic. In fact, you have more strength and options than you think.
First, here is some good news: Craniopharyngioma is not cancer. In medical terms, doctors call it a “benign” tumor. Unlike malignant types, it does not spread to your body like lung cancer. Instead, it stays in one place. However, this tumor brings unique challenges. Because, it sits at the brain’s busiest, most sensitive intersection. Therefore, we pay “special attention” to it. As a result, neurosurgeons know this tumor well. Furthermore, we manage this difficult process with years of experience. Moreover, microsurgical technology is our greatest assistant. Ultimately, we are here to restore your health.
Accordingly, we prepared this comprehensive guide for you. Here, you will find answers to your questions. For example, how do we perform surgery? Do we enter through the nose? Additionally, will your child grow taller? Will you gain weight? Fortunately, we answer these below. Remember, knowledge is power. Thus, knowing your disease makes defeating it easier. So, let’s begin.
What is Craniopharyngioma? Where is it located?
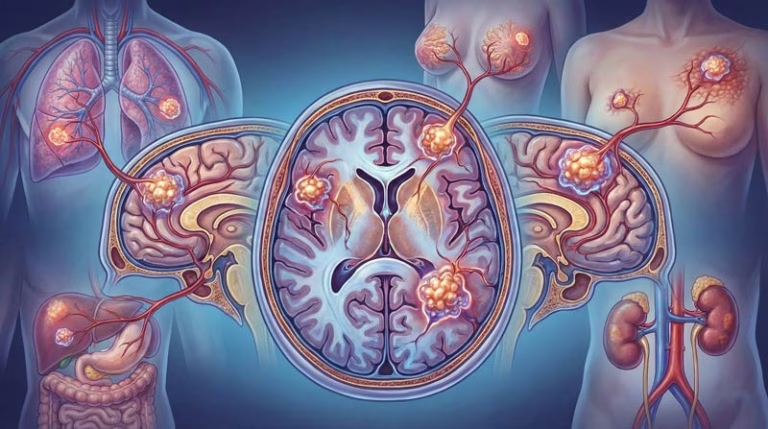
Basically, Craniopharyngioma settles in the brain’s exact center. Due to its position, it grows in the “Sellar Region”. In other words, this spot forms the skull base. Specifically, the tumor sticks tightly to the pituitary gland stalk. As you know, the pituitary gland directs the body’s hormone orchestra. Unfortunately, this tumor grows right above, or sometimes inside, this conductor.
Actually, this region acts as the brain’s most strategic point. Why? Because optic nerves cross here. Furthermore, the brain’s main arteries pass through this area. Most importantly, the “Hypothalamus” resides here. Notably, the hypothalamus controls hunger, thirst, sleep, body temperature, and emotions. Hence, the tumor’s proximity to these structures complicates treatment. Although the tumor is benign, it behaves aggressively. Frequently, it sticks tightly to surrounding tissues. Consequently, surgery becomes a chess game. Therefore, we plan every move carefully.
Statistics show it is a rare tumor. In fact, it makes up only 2-5% of all brain tumors. However, this rate hits 10% in children. Also, it shows a unique age distribution. Primarily, we see it in children aged 5-14. Later, a second peak occurs in adults aged 50-74. Thus, it affects both grandchildren and grandfathers.
Two Different Enemies: Child and Adult Type
Importantly, every craniopharyngioma differs. When looked at under a microscope, we identify two main types. Naturally, we adjust our treatment plan based on the type.
1. Adamantinomatous Type (Childhood): First, we encounter this type most frequently. Generally, it affects children. Structurally, it is complex due to calcifications (ossification). Also, it contains many cystic (fluid-filled) areas. Often, the fluid inside resembles “motor oil.” Specifically, this dark yellow-brown fluid is rich in cholesterol crystals. If leaking occurs, fluid irritates brain tissue. Moreover, these tumors send finger-like projections into the surroundings. Genetically, it links to the “CTNNB1” mutation.
2. Papillary Type (Adult): On the other hand, we usually find this type in adults. Comparatively, its structure is simpler. Generally, it lacks calcification. Instead, it has fewer cysts and resembles a solid piece of meat. In addition, it adheres less to surrounding tissues. Therefore, complete surgical removal is often easier. Genetically, it carries the “BRAF V600E” mutation. Detecting this is vital, because new smart drugs may work for this type.
Symptoms: Vision, Hormones, and Headache
Usually, these tumors grow slowly. Consequently, the brain adapts to the growth for a while. Therefore, symptoms progress insidiously. Very often, they develop over months or years. However, the body sounds an alarm when the mass reaches a critical size.
1. Vision Loss: Is Your World Narrowing?
When the tumor grows upward, it presses on the optic nerves. As a result, this pressure causes a typical blindness: “Bitemporal Hemianopsia”. Simply put, you lose side vision. Specifically, you cannot see your right and left when looking straight. For example, you miss side mirrors while driving or bump into door frames. Also, visual acuity drops, and colors fade. Similarly, children cannot see the board, and grades drop. Unfortunately, without early diagnosis, this loss becomes permanent.
2. Hormonal Collapse: The Body’s Balance Fails
Eventually, crushing the pituitary gland stops hormone production. This leads to severe consequences:
- Growth Hormone Deficiency: For instance, we see this most in children. The child remains short. Clothes still fit after a year. Shoe size stays the same.
- Gonadotropin (FSH/LH) Deficiency: Puberty delays. Adults lose sexual desire. Additionally, men face erectile dysfunction. Women experience menstrual irregularity or menopause.
- TSH (Thyroid) Deficiency: Metabolism slows. The patient feels cold constantly. Weight gain occurs. Also, skin dries out. Fatigue prevents simple tasks.
- ACTH (Cortisol) Deficiency: Most dangerously, the body cannot handle stress. Blood pressure drops. Sudden fainting happens. It carries a vital risk.
- Diabetes Insipidus: A damaged pituitary stalk cannot secrete ADH. Thus, kidneys fail to hold water. The patient drinks 5-10 liters daily. They wake up 10 times at night. Thirst and insomnia exhaust the patient.
3. Increased Intracranial Pressure (Hydrocephalus)
If large tumors block the brain’s water channels, Cerebrospinal fluid (CSF) accumulates. Consequently, intracranial pressure rises. Typically, the patient wakes with a severe headache. Unfortunately, painkillers do not help. Then, projectile vomiting starts. Also, eye ground swells (papilledema). Finally, advanced stages bring drowsiness and coma.
Hypothalamic Syndrome and Obesity Risk
Above all, hypothalamic damage worries us most. Because, the hypothalamus acts as the brain’s “satiety center.” Thus, tumor invasion or surgical damage here causes “Hypothalamic Obesity.”
Clearly, this is not ordinary weight gain. First, the patient loses the feeling of fullness. Even after a meal, the brain says “I am hungry”. Also, the metabolic rate drops. Seemingly, even water adds weight. Consequently, rapid, uncontrolled weight gain follows. Moreover, rage attacks and excessive sleepiness occur. Therefore, we changed our surgical principle. Now, we do not sacrifice the hypothalamus for total tumor removal. Instead, we leave a piece if necessary to protect quality of life.
How Do We Diagnose? MRI and CT Roles
Initially, patient complaints make us suspicious. Then, we confirm the diagnosis with imaging.
MRI (Magnetic Resonance): This is the gold standard. To clarify, we perform a contrast-enhanced brain MRI. We see cystic and solid parts clearly. We map vessel relationships. Ultimately, MRI guides our surgery plan.
CT (Computed Tomography): These tumors often calcify. While MRI misses calcification, CT shows bone and lime perfectly. So, we use CT to confirm the diagnosis.
Eye Examination: We test the visual field. This documents optic nerve damage.
Hormone Panel: We check all hormone levels via blood tests. We replace deficiencies before surgery. This ensures anesthesia safety.
Surgical Treatment: Nasal Route or Open Surgery?
Surgery is the first and most important step. Our goal: Remove the tumor safely, relieve optic nerves, and save the pituitary. To achieve this, we use two main methods:
1. Endoscopic Endonasal Approach (Nasal Surgery)
We prefer this method globally and in our clinic. It works best for midline tumors.
The Procedure: First, we enter nostrils with a thin camera (endoscope). Then, we open the skull base bone. Finally, we reach the tumor from below.
Advantages: No head incision. We do not retract brain tissue. We see the tumor-hypothalamus attachment perfectly from below. This allows safe separation.
Reconstruction: We close the hole with a nasal mucosal patch (flap). This prevents fluid leakage.
2. Transcranial Approach (Open Brain Surgery)
We choose this for large side-growing tumors or hard, calcified ones.
The Procedure: Initially, we make a hidden scalp incision. Next, we lift a small bone lid. Carefully, we glide between brain folds under a microscope to reach the tumor. Experienced hands make this method safe and effective too.
Surgeons decide the method based on tumor location, shape, and nasal structure. Sometimes, both options apply.
Cyst Treatments and Ommaya Reservoir
Some tumors form giant cysts. Aged or weak patients may not withstand major surgery. In these cases, we install an “Ommaya Reservoir”. This coin-sized reservoir sits under the skin. A thin tube connects it to the cyst. When needed, we drain fluid via a needle. Also, we inject tumor-shrinking drugs (Bleomycin or Interferon). Effectively, this method spares the patient from major surgery.
Radiation Therapy: Gamma Knife and Proton
We avoid forcing removal if the tumor sticks to the hypothalamus. We leave a small piece. We call this “Subtotal Resection.” Subsequently, we use radiation.
Gamma Knife Radiosurgery: This is scalpel-free surgery. Basically, we focus high-dose radiation on the tumor in one session. The patient goes home the same day. Side effects remain low. It stops growth in 90% of cases.
Proton Therapy: We prefer this for children. This advanced tech minimizes radiation damage to healthy tissues. Thus, we protect the child’s brain development.
Recovery Process: Intensive Care and Hormones
Surgery ends, but the process continues. Therefore, recovery needs patience.
Intensive Care: You stay one night usually. We monitor “Fluid and Salt Balance” closely.
Sodium Fluctuations: Salt levels may rise and fall after surgery. We call this a “triphasic response.” So, frequent blood tests track this.
Diabetes Insipidus (DI): You might drink and urinate excessively for a while. Nasal sprays or pills control this. It usually resolves, but can become permanent.
Cortisone: The body needs steroid drugs during stress. However, never stop these without doctor orders.
Returning Home: Hospital stay lasts 4-6 days. Afterwards, you return to normal life slowly at home. Regular checks adjust hormones. You can live an active life with regular medication.
Frequently Asked Questions (FAQ)
Is craniopharyngioma surgery risky?
Every brain surgery carries risks. However, experienced centers perform this with low risk. Main risks include hypothalamic damage (weight gain), vision loss, and hormone deficiency. Surgeons use “safe surgery” principles to minimize these.
How long does surgery take?
It lasts 4 to 8 hours depending on size and adhesion. This seems long. However, surgeons prioritize precision, not speed. We work patiently, millimeter by millimeter, to protect the brain.
Does the tumor recur?
Yes, these tumors love to recur. Unfortunately, they come back in 10-20% of cases even after total removal. Leftover pieces increase risk. Therefore, we do MRIs every 3-6 months initially. Gamma Knife stops early recurrences easily.
Will my child grow and enter puberty?
Treatment exists even if the pituitary fails. Specifically, endocrinologists start “Growth Hormone” shots. Then, children reach their genetic height potential. Sex hormone supplements allow normal puberty and future fertility.
When can I return to work or school?
We suggest 3-4 weeks of home rest. Wounds heal and hormones settle during this time. Finally, you can return after a month if you feel good. Avoid heavy sports for 2-3 months.
Is this disease genetic?
No, it is not hereditary. Actually, it is a developmental accident in the womb. Siblings or relatives do not face higher risk.
Note: This content is for information only. It does not replace medical advice. Consult an expert neurosurgeon for accurate diagnosis. Early diagnosis saves lives.
Ready to Take the Next Step?
Schedule your consultation with Dr. Albayrak today and start your journey towards better health.